Navigation Menu:
D. Hyperbaric Oxygen Therapy and Diabetic Foot Ulcers
E. Application of Hyperbaric Oxygen Therapy to Chronic Wounds
Introduction to Diabetes
Diabetes is defined as a group of diseases that result in too much sugar in the blood, and is also referred to as high blood glucose. In 2015, 30.3 million Americans, or 9.4% of the population had Diabetes[1].
The rates of diagnosed diabetes in adults by race/ethnic background are [1] :
- 7.4% of non-Hispanic whites
- 8.0% of Asian Americans
- 12.1% of Hispanics
- 12.7% of non-Hispanic blacks
- 15.1% of American Indians/Alaskan Natives
When a person eats food that contains carbohydrates, it is broken down in the stomach and digestive system into glucose, a type of sugar. Glucose from food is vital as it is what gives us energy.
system into glucose, a type of sugar. Glucose from food is vital as it is what gives us energy.
Foods containing carbohydrates include starchy foods, sugary foods, milk, some dairy products, and fruit. The glucose then moves into the bloodstream and the body detects that the blood glucose level is rising. In response to that the pancreas, which is a small gland that sits just below the stomach, starts to release a hormone called insulin and this insulin helps our body get the energy from the food we eat. The blood stream then takes the glucose and the insulin to every cell in our body that needs it.
To make this easier to understand let’s discuss muscle cells. At the muscle cell, it is insulin that allows the glucose to get into the cells where it can be used for energy. It’s much like insulin is a key unlocking the door to the cells so the glucose can get in. That way, the blood glucose levels start to drop. However, the blood glucose level can be topped up at any point by the liver releasing extra glucose that it has stored. The blood glucose rises again, and again. The pancreas produces more insulin to move with that glucose through the bloodstream to the muscle cells. This insulin open the doors, and lets the glucose in.
The body functions best with the blood glucose at an optimum level. It doesn’t like it if the blood glucose rises too high. Normally, there’s a cycle within the body which balances out the glucose and the insulin level. This is achieved through the food that you eat, and the functions of the pancreas and liver. However, in some people the system doesn’t work properly and they develop diabetes.
Diabetes remains the 7th leading cause of death in the United States in 2015, with 79,535 death certificates listing it as the underlying cause of death, and a total of 252,806 death certificates listing diabetes as an underlying or contributing cause of death[1].
There are two main types of diabetes :
- Type 1 Diabetes
- Type 2 Diabetes
Type 1 Diabetes
When a person has Type 1 Diabetes the body isn’t making any insulin at all. This is because of an autoimmune response whereby the body has destroyed the insulin producing cells in the pancreas. It is not entirely known why this happens in some people and not in others. Type 1 Diabetes accounts for about 5 percent of all cases of diabetes [1]. It is most often found in people under 40 and it is by far the most common type of diabetes found in childhood. In 2015, approximately 1.25 million American children and adults have type 1 diabetes. [1]
With Type 1 Diabetes, the carbohydrate containing food is turned into glucose as normal. That glucose then moves into the bloodstream. Normally the body would produce insulin to let that glucose into the cells but in Type 1 Diabetes there is no insulin being produced, so the glucose can’t get into the body cells at all. This causes the level of glucose in the blood to rise. The body tries to lower the level of glucose using the kidneys. This is why people who have undiagnosed Type 1 Diabetes tend to go to the bathroom a lot to pass urine. As the kidneys filter the glucose out of the blood, they take a lot of water with it. As a result, the person with diabetes can get very thirsty. The urine contains a lot of glucose, and that creates an environment where it’s quite easy for bacteria to thrive. Because of this, it’s also quite common to get thrush, or genital itching.
In the same way, the blood contains a high level of glucose as well, so more bacteria than usual will

tend to breed in flesh wounds. As a result, they might be slow to heal. Glucose can also build up in the lens at the front of the eye, causing the liquid in the lens to become cloudy. That can mean that some people with undiagnosed Type 1 Diabetes can have blurred vision. Because the glucose can’t get into the cells to be used for energy, a person with undiagnosed Type 1 Diabetes is going to start feeling very tired, lethargic, and unable to go about their normal daily routine. With that said, the body still needs an energy source in order to work properly, so it starts to break down its fat stores and that can lead to weight loss.
The main symptoms of Type 1 Diabetes [2]:
- Excessive urination
- Thirst
- Thrush or genital itching
- Slow healing of wounds
- Blurred vision
- Tiredness
- Weight loss.
These symptoms generally happen quite quickly, often over a few weeks, and can be reversed once the diabetes is treated with insulin. Today, insulin is most commonly delivered using an insulin pen.
Type 2 Diabetes
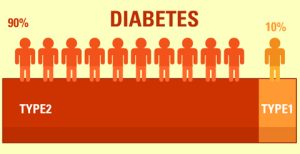
Type 2 Diabetes accounts for about 90% of all cases in the population[1]. It’s most common in the over forty age group in the white population, and in the over twenty five age group in the black or South Asian population. Type 2 Diabetes is a little more complex, because there are more processes at work. Either the body isn’t producing enough insulin, or the insulin it is producing, isn’t working properly. This can be caused by being overweight, because a buildup of fat can keep insulin from doing its job properly. However, it can also happen in people of a healthy weight.
In Type 2 Diabetes, the carbohydrate containing food is broken down into glucose in the stomach and digestive system as normal. That glucose then moves into the bloodstream. The pancreas starts to produce insulin, which moves with the glucose through the bloodstream, to all of the body’s cells that need glucose for energy.
However, the glucose can’t always get into the cells, because the locks to the cell doors have become furred up with fat deposits. This prevents the insulin from being able to open the cell doors properly. The level of glucose in the blood continues to rise, and in response to this, the pancreas produces even more insulin. The blood glucose levels continue to rise and the insulin levels continue to rise. This situation is further complicated by the cells who are desperate for energy, sending out emergency signals to the liver to release stored glucose.
The blood glucose level rises, and the pancreas produces more and more insulin
until it can’t cope anymore. The pancreas eventually wears out. As with Type 1 Diabetes, the symptoms of Type 2 Diabetes are excessive urination, thirst, thrush, genital itching, slow healing of wounds, blurred vision, tiredness, and weight loss. The symptoms for Type 2 Diabetes come along very slowly, and some people don’t have any symptoms at all. For these reasons, people can live with Type 2 Diabetes for up to ten years before they realize that they have it.
Type 2 Diabetes can be treated in a number of different ways. Initially, it may be sufficient to make changes to the food you are eating and exercise more. One would also want to lose any excess weight. However, Type 2 Diabetes is a progressive condition, and most people will need some form of medication to treat it.
Risk factors for developing prediabetes or type 2 diabetes [2] :
- Overweight or obesity
- Age 45 and older
- Have a parent, brother, or sister with type 2 diabetes
- Are physically active less than 3 times per week
- Have ever had gestational diabetes (diabetes while pregnant) or given birth to a baby weighing more than 9 lbs.
- American Indians/Alaska Natives are twice as likely as whites to have diabetes.
Diabetic Foot Ulcers
A diabetic foot ulcer is a very dangerous skin breakdown, opening the door to bacterial infection and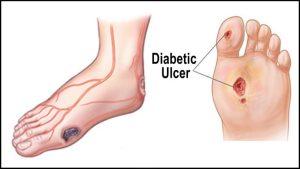 possible amputation of the affected foot. Most skin ulcers occur at the bottom aspect of the feet as a result of these areas being subject to weight bearing. The most prevalent areas affected by the skin breakdown include bottom aspects of the feet, mainly heels and the ball of the foot, and of the most prominent of the most hyper contracted toes.
possible amputation of the affected foot. Most skin ulcers occur at the bottom aspect of the feet as a result of these areas being subject to weight bearing. The most prevalent areas affected by the skin breakdown include bottom aspects of the feet, mainly heels and the ball of the foot, and of the most prominent of the most hyper contracted toes.
The poor peripheral blood circulation of people with diabetes, sometimes complicated with poor distal nerve conduction and protection, sooner or later will weaken the ability of the skin of the affected feet to regenerate and heal. Ulcers will develop because the feet are far away from the heart, the very last to receive the blood nutrients as well as the very first to suffer from an impaired blood circulation. The reduced blood flow to the foot results in slow healing and low sensitivity. As a result, diabetic foot ulcers are responsible for more hospitalizations than any other complication associated with diabetes[2].
An ulcer is a breakdown in the skin and is a chronic problem. It’s not as simple as a cut or a scratch, which typically heals uneventfully. This is a chronic problem that develops slowly over time. Typically, an ulcer will occur in an area of your foot where people would typically develop a callus such as the ball of your foot, the tip of your toe, the inside of your big toe, or any high pressure area where you might develop a callus. The difference is that the calcite is then progressed to actually break down the deeper layer of the skin.
Three things must be in place for this ulcer to develop. First, one has to have neuropathy. Neuropathy prevents a person from being able to feel the changes taking place in the foot to let you know that the skin is about to break down. These types of changes would include the heat of pain or swelling, but neuropathy will prevent you from feeling these sensations.
The next necessary occurrence is pressure. There is pressure simply from walking day to day. Often times, the patient stepped on something on the bottom of the foot and it caused a puncture breakdown in the skin.
The third necessary presence for the forming of a diabetic foot ulcer is diabetes. The puncture breakdown progresses to an ulceration when diabetes prevents the foot from healing properly. This happens because diabetes affects the blood flow to your foot, which then prevents the patient’s body’s own growth factors or healing enzymes to present in the wound site. This prevents it from healing in a normal fashion. Diabetes also suppresses one’s immune function preventing a patient from developing an appropriate immune response to fight off any infectious processes that might be present in the wound site.
As a diabetic foot ulcer develops, it will often become red and will have a large amount of callus formed around the margin of the wound. At first when it is noticed, it may be covered by a large portion of callous, but it can be felt. You can notice that there is either fluid draining from the site which might be pus, blood, a clear yellow fluid called plasma, or serous fluid. All of these are indications that something more serious than an inflamed callus is going on.
This condition can also progress to the point to where the callus falls off of the wound site and you have an open red wound.
Hyperbaric Oxygen Therapy and Diabetic Foot Ulcers
Normally, the air that we breathe is a mixture of gases, with oxygen accounting for about 21% of this mixture. However, during hyperbaric oxygen therapy, one breathes 100% oxygen, while under pressure, causing the oxygen to dissolve into the plasma in the blood. This is known as hyperoxia. It also allows for higher concentrations of oxygen to flow through the body, including the areas with limited blood flow. This results in improved healing.
Hyperbaric oxygen therapy, otherwise known as HBOT, increases the oxygen concentration of the blood. Due to the increase in oxygen, new blood vessels develop in the affected areas. This improves the effectiveness of antibiotics and the body protective system response or immune response.
Hyperbaric oxygen therapy (HBOT) has been promoted as an effective treatment for diabetic foot ulcers[3].
Gas gangrene and Necrotizing Fasciitis are both caused by harmful bacteria that can cause severe infection and destruction of the skin and muscle. HBOT increases the oxygen delivered to these areas which kills the harmful bacteria. It also enhances the activity of white blood cells and certain antibiotics. These all result in rapid healing. The demonstrated effects of Hyperbaric Oxygen Therapy on diabetic foot ulcers include [4]:
- Improvement of wound tissue hypoxia
- Enhanced perfusion
- Reduced edema
- Downregulating Inflammatory cytokines
- Promotion of fibroblast proliferation
- Collagen production
- Angiogenesis
Application of Hyperbaric Oxygen Therapy to Chronic Wounds
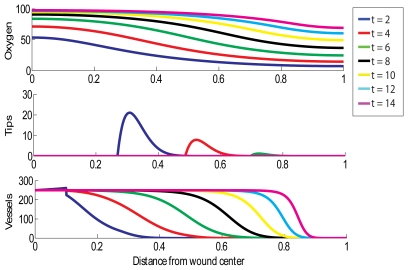
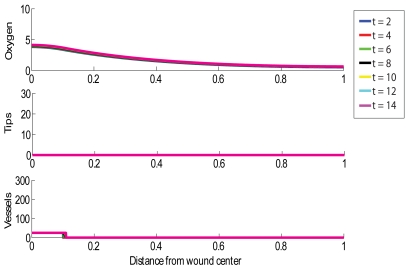
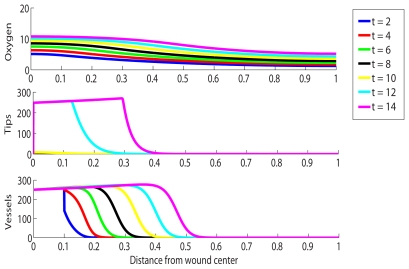
Below, we will show three models. Each displays a different scenario of an acute wound of 2cm in length and how it can heal in differing environments.
The top third of each chart labeled “oxygen” shows oxygen tension measured in (mmHg). The middle segment labeled “tips” shows tip density measured in capillaries/cm^2.
The segment labeled “vessels” in each graph shows blood vessel density measured in vessels/cm. In all of these graphs, “t” is equal to the number of days since the injury occurred.
This first model simulates the wound healing successfully without HBOT exposure. In this “normal” situation, the wound is almost completely reoxygenated within 2 weeks. This is indicated by the purple line (14 days) having 100% oxygen tension at the wound center.
This second model shows the same 2cm wound, but in this simulation the wound is chronic, is receiving no treatment, and is not healing. Notice that throughout the simulation, the oxygen tension does not rise at all. There is no significant change over time, indicating that no healing is taking place.
This third model simulates the same 2cm chronic wound with the help of hyperbaric oxygen therapy to aid in it’s healing. From this simulation we notice that the capillary tip density in the chronic wound reaches elevated levels under treatment and that healing is initiated quickly.
References :
[1] American Diabetes Association, http://www.diabetes.org/diabetes-basics/statistics/
[2] CDC (Centers for Disease Control and Prevention), https://www.cdc.gov/diabetes/basics/quick-facts.html
[3] Baroni G, Porro T, Faglia E, Pizzi G, Mastropasqua A, Oriani G, Pedesini G, Favales F: Hyperbaric oxygen in diabetic gangrene treatment. Diabetes Care 1987; 10: 81– 86 [PubMed]
[4] Gill AL, Bell CN: Hyperbaric oxygen: its uses, mechanisms of action and outcomes. QJM 2004; 97: 385– 395 [PubMed]